Instructions:
-
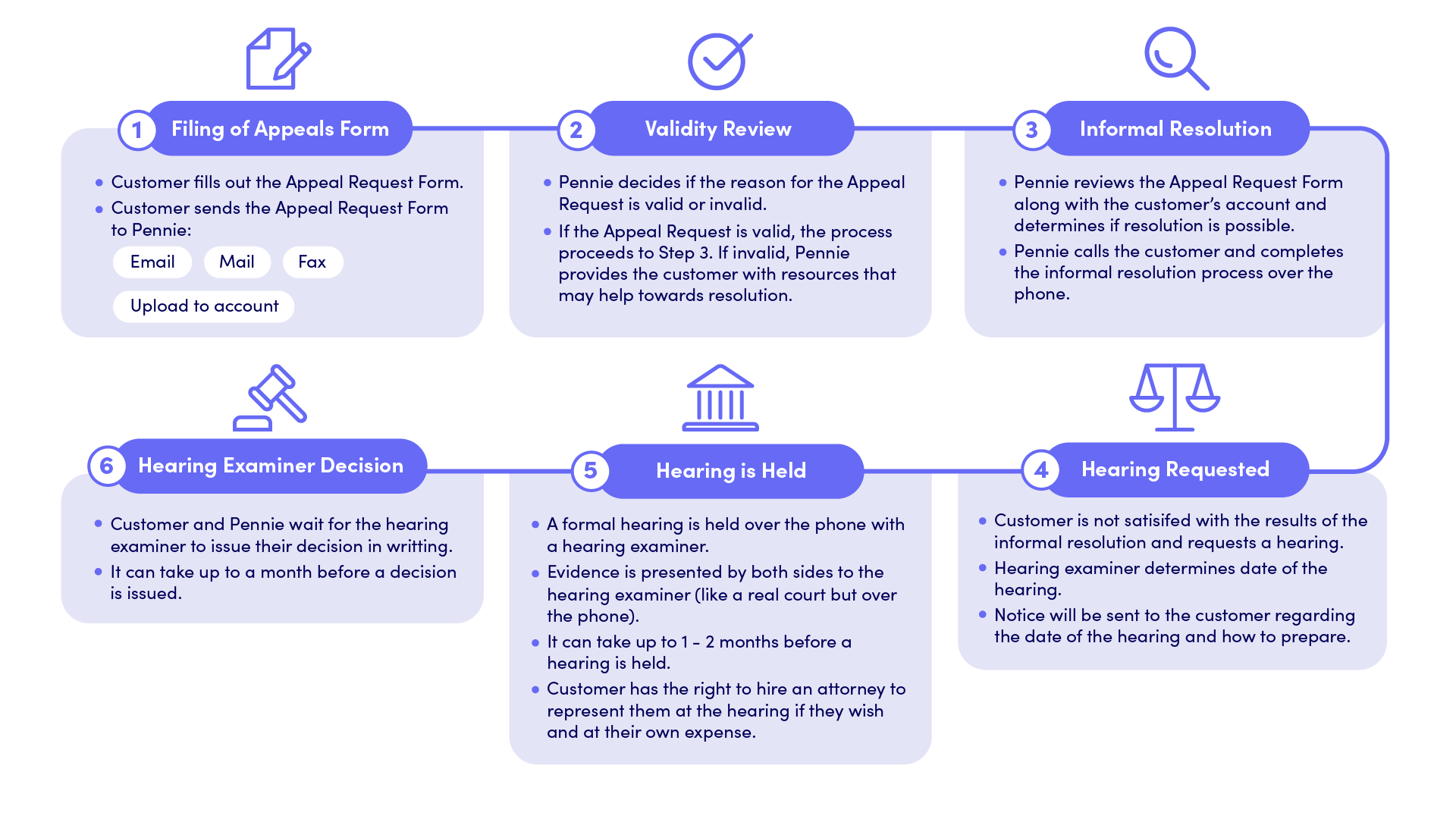
- Download and complete Pennie’s Appeals Request Form or en Espanol.
- Attach supporting documentation.
- Return the completed form to Pennie.
Email: appeals@pennie.com
Fax: 717-232-2226
Mail: Pennie Appeals, P.O. Box 2008, Birmingham, AL 35203
Note: You can add someone to file the appeal and speak with Pennie on your behalf on pages 11 and 12 of the Appeal Request Form.
You may request a faster appeal if you have health risks.
All appeals from Pennie actions are governed by 45 C.F.R. §§ 155.500-155.555 and the General Rules of Administrative Practice and Procedure, 1 Pa. Code Part II, Chapters 31-35.
If this is your first attempt to reach Pennie, you can file a complaint. This may be a faster, easier way to get help.
-
-
- Call Pennie at 844-844-8040 to request a compaint ticket be created (or)
- Log into your Pennie account.
- From your Pennie Dashboard, select “My Tickets”.
- Create a new ticket.
- Add supporting documents and click “Submit”.
- Follow-up or add comments to your ticket anytime via “Ticket History”.
-
Please allow 30 days for Pennie to review your complaint and contact you.
The Appeals Process